reconstructing a journey
This page chronicles a journey from the moment of my cancer diagnosis through the start of the treatments that led to my remission. Please note this isn’t a medical manual, nor is it a benchmark for how quickly or slowly a cancer journey should unfold. It is simply my story.
As part of my cancer archive, this is a personal reconstruction of some events. My goal is to remember the long road I traveled, allowing myself to regain control, while hopefully helping someone else navigating the overwhelming experience of a (breast) cancer diagnosis.
profound comfort can be found in knowledge,
and immense power in the ability to access it
how does this work
Explore the timeline below to see the pivotal moments that started in October 2023, the month I learned I had triple-negative breast cancer. You can click on each date (each dot) to uncover the (medical) records from that day. These files, images, and notes were the individual pieces that formed the larger picture of my diagnosis. Please note that you cannot scroll these images as you would do in a regular user experience. This is on purpose: I want you to open each data point on its own, digest it, if possible, close it, and then move on to the next one.
If you want to know more about how I gathered and/or generated this data, go over here.
This timeline spans nine days over the course of three weeks, from the day of my first breast ultrasound to the day of my first chemotherapy session.
The other part of the journey - the one that led to my remission - doesn’t follow a linear path and I am not able to reconstruct it with the same approach, so I am still figuring out how to do that.
October 17, 2023


first echography
On October 17th 2023 I went to the hospital for an echography; the radiologist asked me almost immediately if they could perform a biopsy. So they stuck a needle in my breast and took out a few tissue samples. It was painful as hell and I ended up crying, confused, and trembling on the bed. The doctor asked me why I went alone for a check of this entity. Well, I didn’t know better, but there was my first lesson:
if you can, bring someone with you to medical appointments
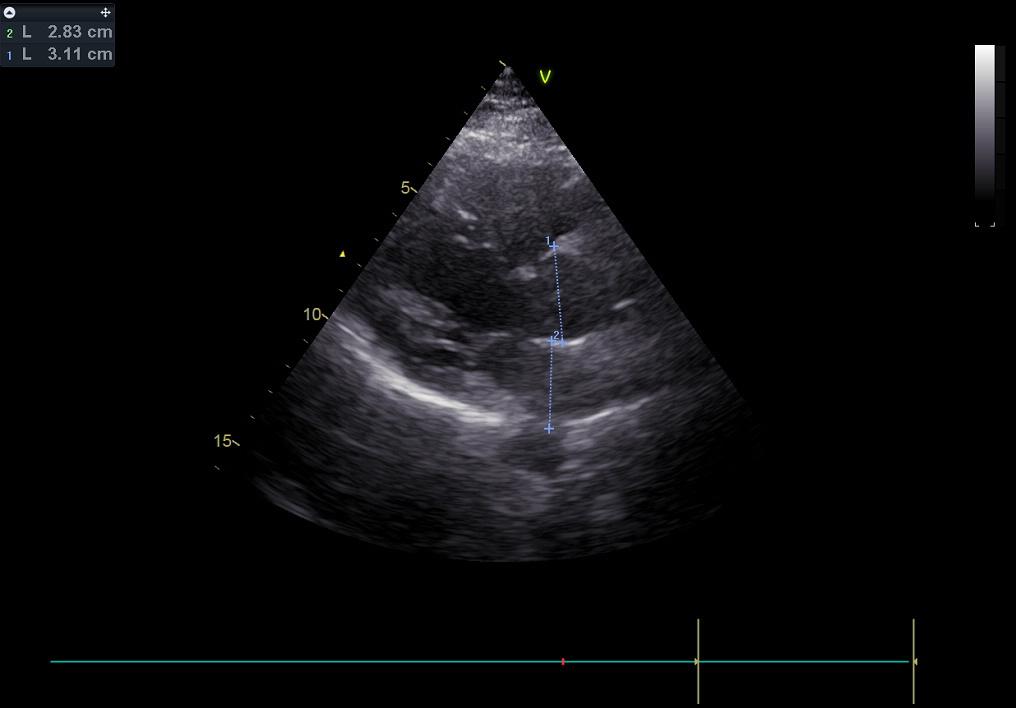
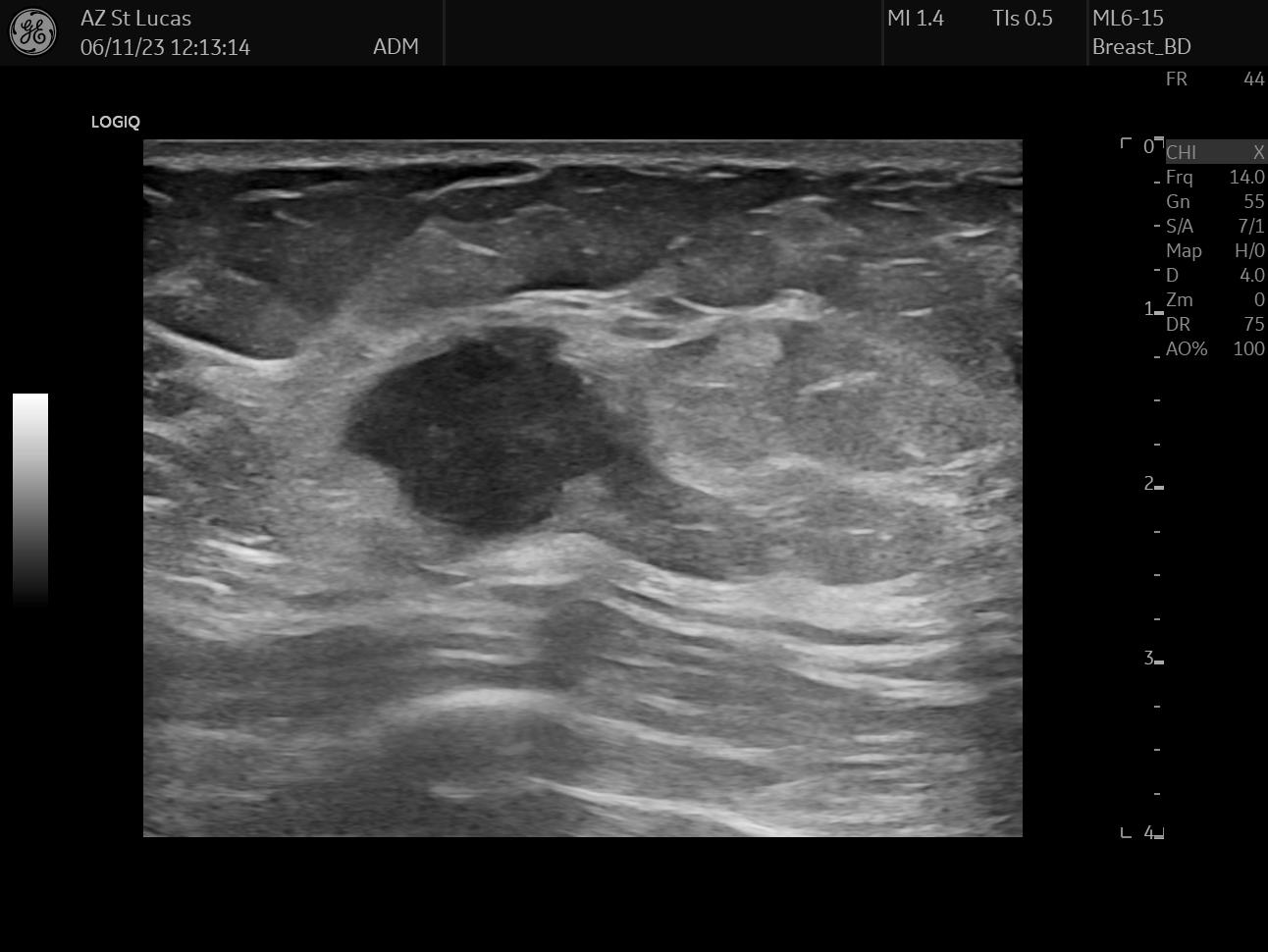
The files I chose for this day are two scans from the echography, they both clearly show the lesion; the second picture also shows the measurements the radiologist took.
October 20, 2023
mammography, first visit with gynecologist: I was diagnosed
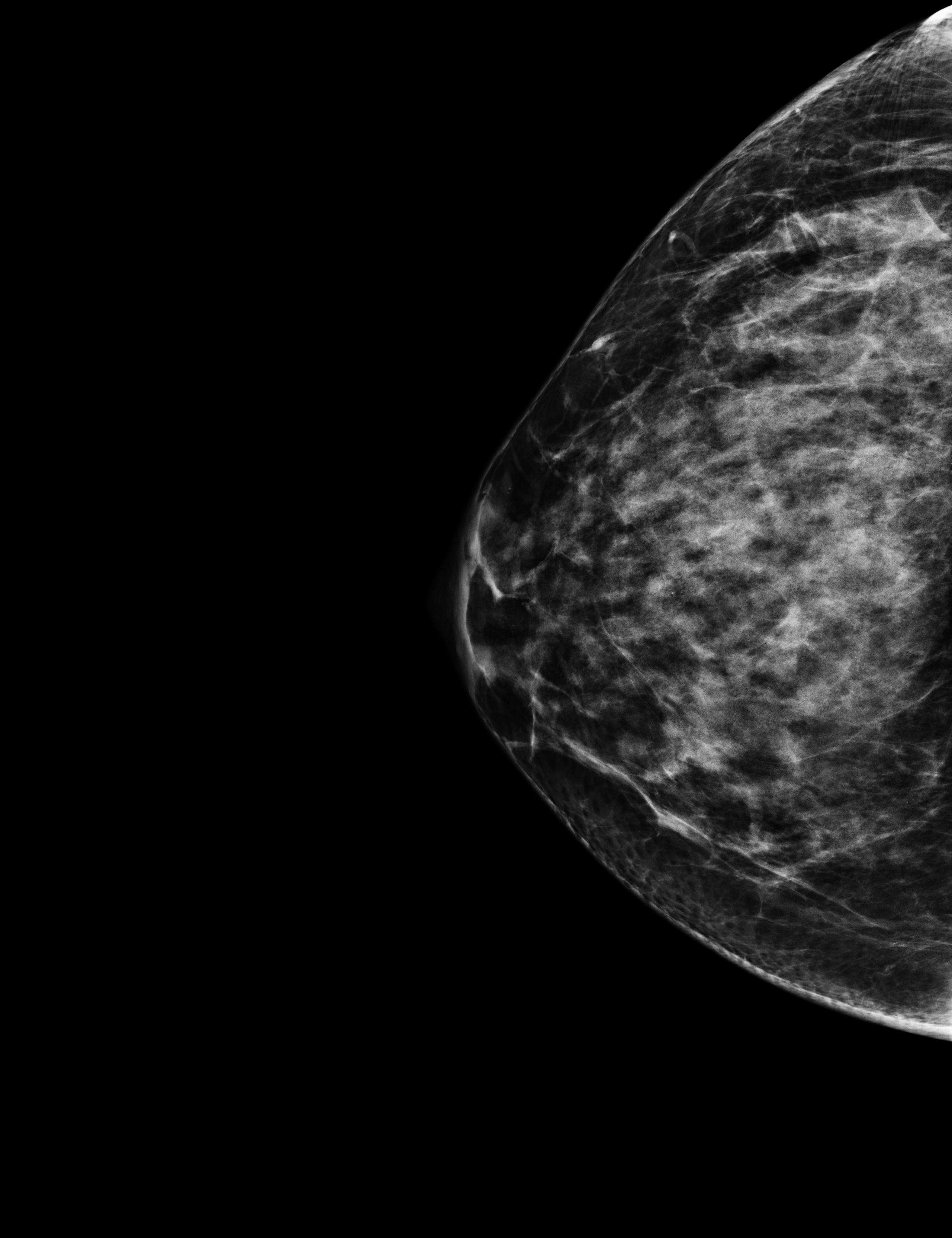
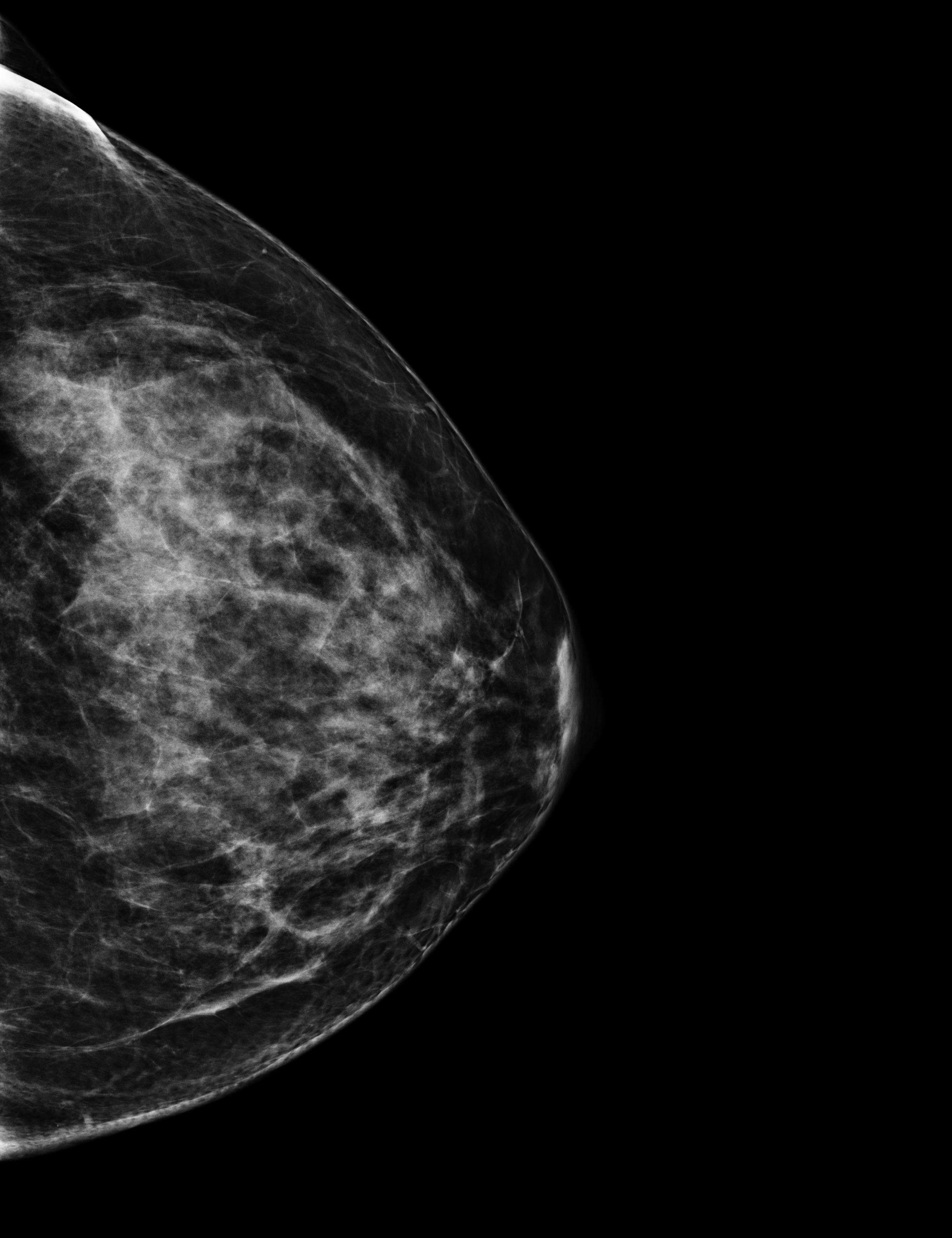
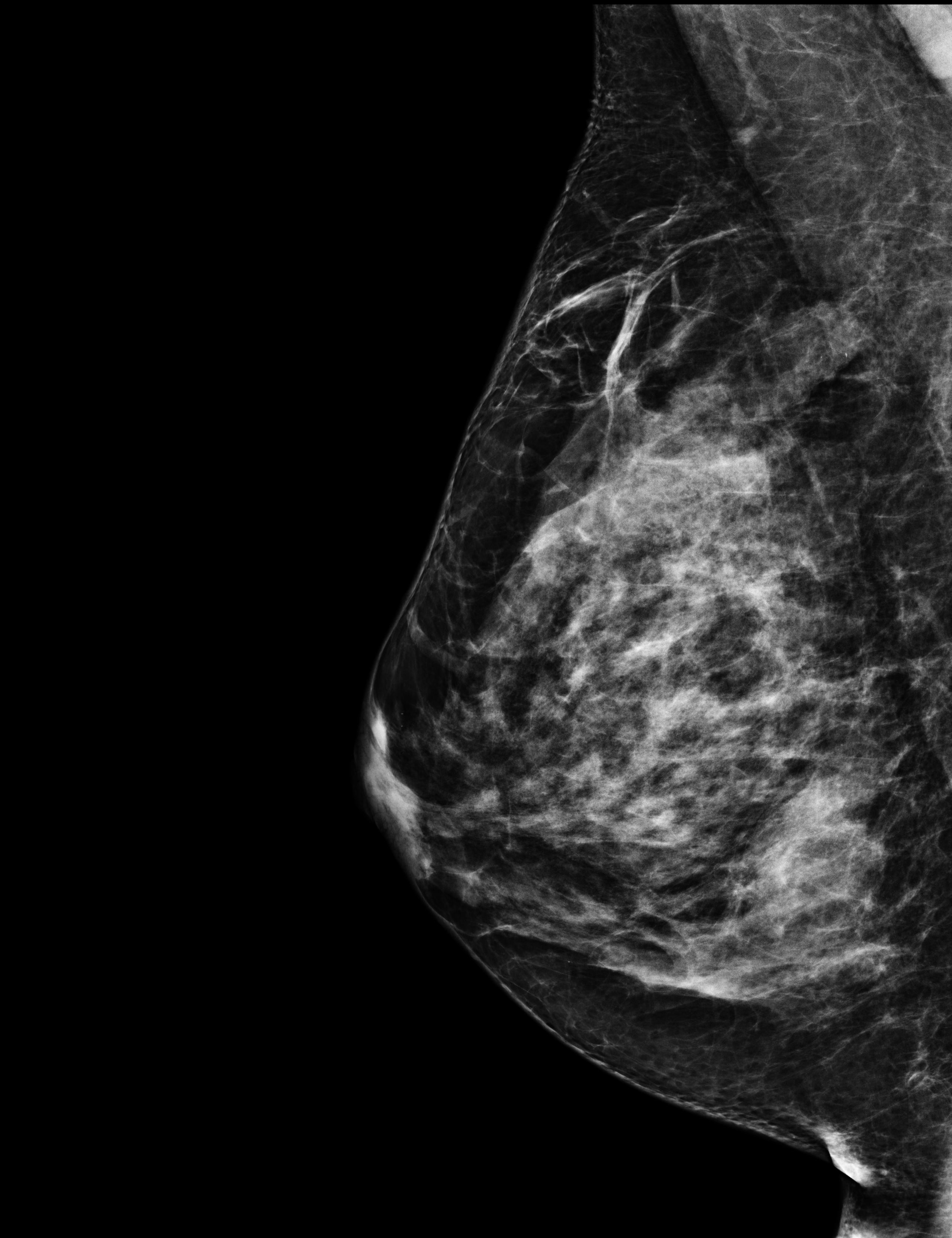
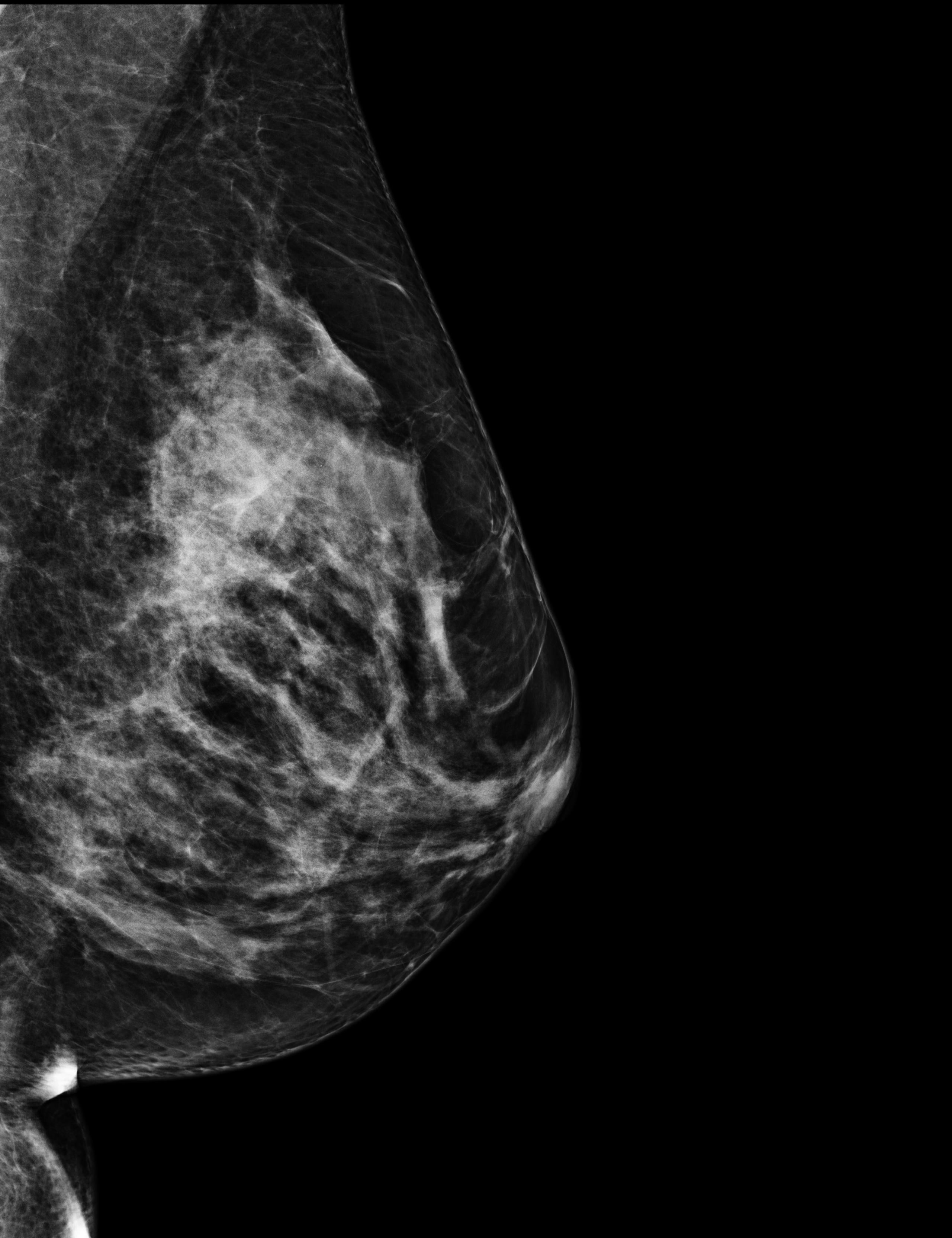
The radiologist that saw me on October 17th, booked me a mammography for 3 days later. I had never done this exam before, and it was very painful, especially because my breast was still suffering from the biopsy. But a mammography can highlight things that an echography cannot, so it was necessary. In the meantime, the results of my biopsy came in, and there was no doubt: “it’s cancer, a breast carcinoma, and unfortunately a triple negative one”, said the doctor.
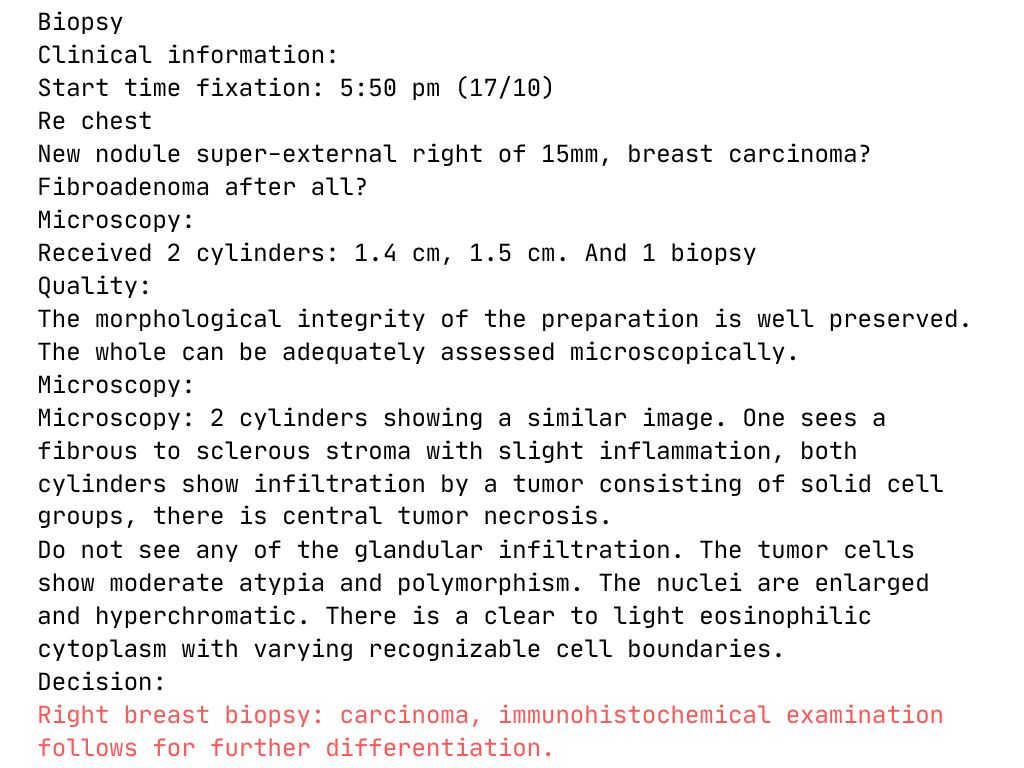
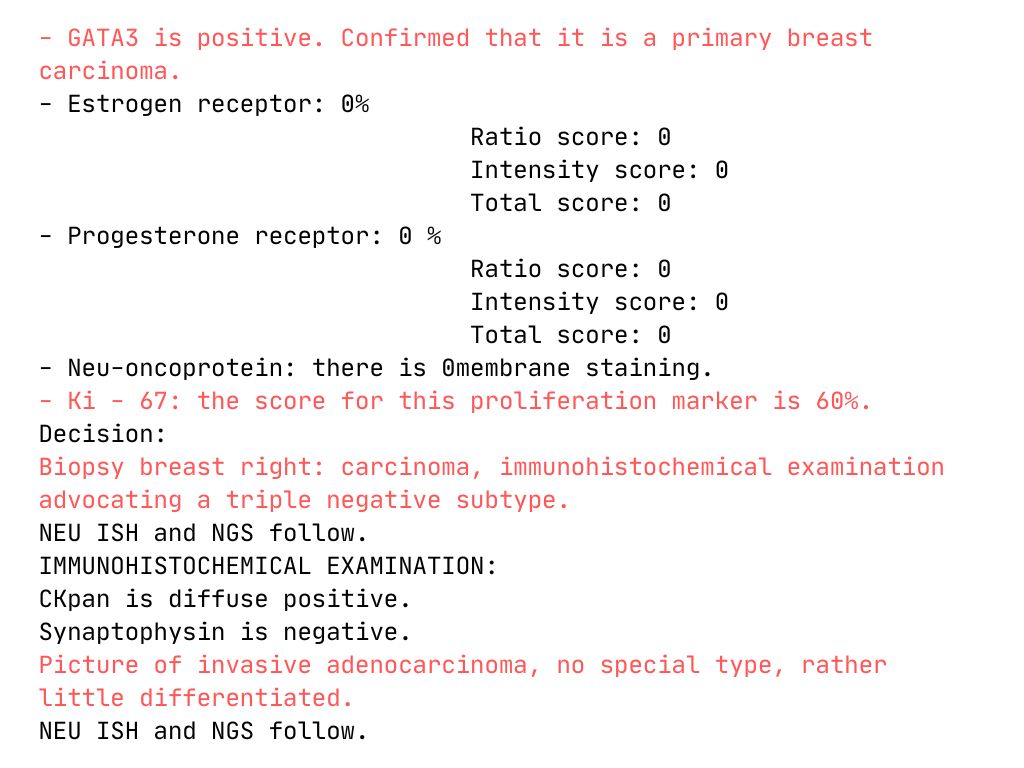
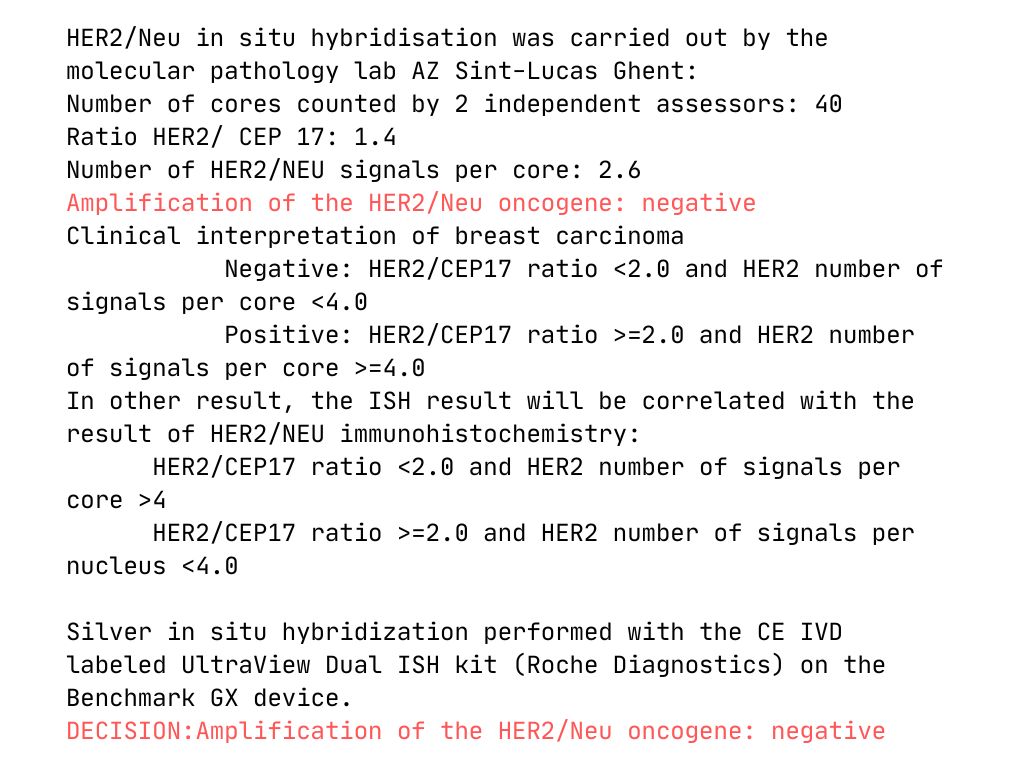
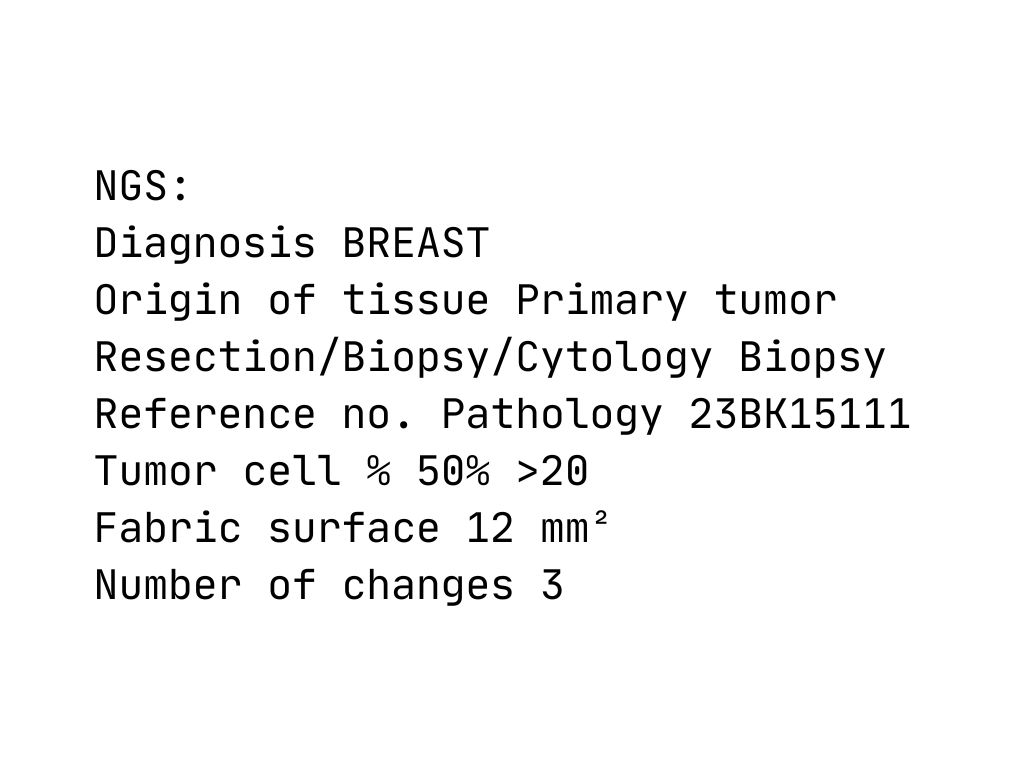
The data I chose for this event are the four scans of the mammography and a revised version of the biopsy results. The biopsy analysis started on 2023-10-17 at 5:50pm, and it kept being updated until 2023-11-01. I have highlighted in red the medical decisions (besluit, in Dutch). At the end you’ll also find a single value, the level of the CA 15-3 tumor marker in my blood. Keep it in mind: it will come back later on.
first chat with a breast nurse
The gynecologist explained the therapy plan and the additional exams that needed to happen as soon as possible. I was not alone, this time around, and I am forever grateful about it: I didn’t understand all of it, to be honest, too caught up in a whirlwind of thoughts, fears, questions. I was sent to the breast clinic, where a breast nurse was ready to talk to me. I was given a folder and a box: everything I needed to know was in there. I just couldn’t stop crying.
There was a book inside the box. A book on living with and after breast cancer. I have read it all. Back and forth. I still have it at home, in the living room library.
October 23, 2023
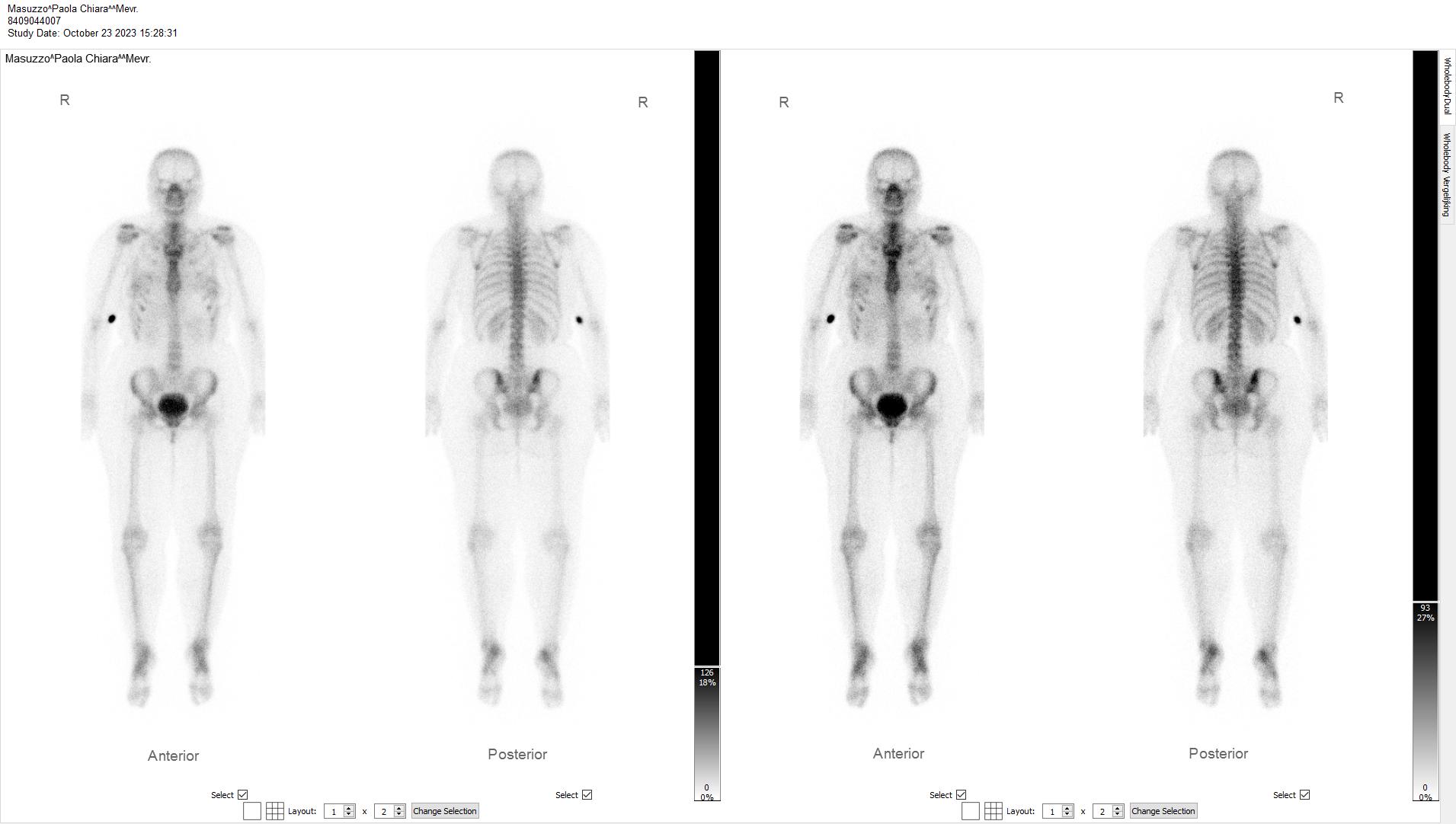

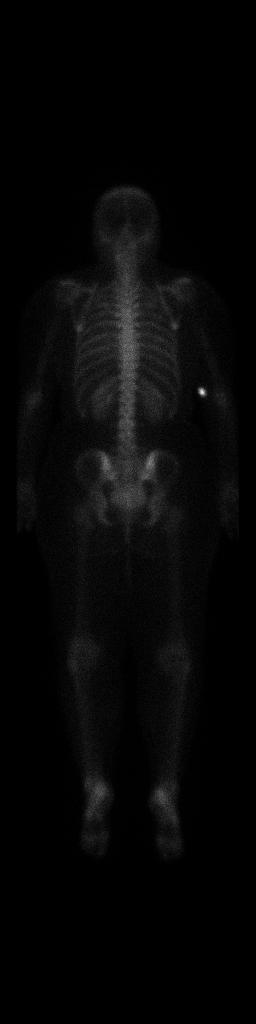
bone scan scintigraphy
On October 23rd 2023 a series of medical exams started for me. The overall goal was to exclude cancer metastases in my body and to understand a bit better the general status of the disease. I started with a bone scan scintigraphy. It went down more or less like this: I was injected a radioactive substance, then sent home for a few hours, where I was allowed to eat and I had to drink a lot of water, the more, the better. For the exam to take place, the bladder needs to be empty (a full bladder can obscure the pelvis and surrounding pelvic bones), so they asked me to pee right before getting on the table. The exam lasted around 45 minutes, which seemed an eternity as in the middle of it I realized I had to pee again, and I obviously couldn’t. Also, the camera moved very very close to my face without touching it: overall, an horrible experience. A few days later I had the results: the medical report stated that there were “no arguments for bone metastases”.
You can see some points in my body lighting up, but apparently this was not related to cancer. Fun fact: I remember the technician in the room asking me to try and focus and not piss myself on the table (because apparently this can happen). They said something like: “there’s no shame in it, but I really don’t want you to have to do this all over again.”
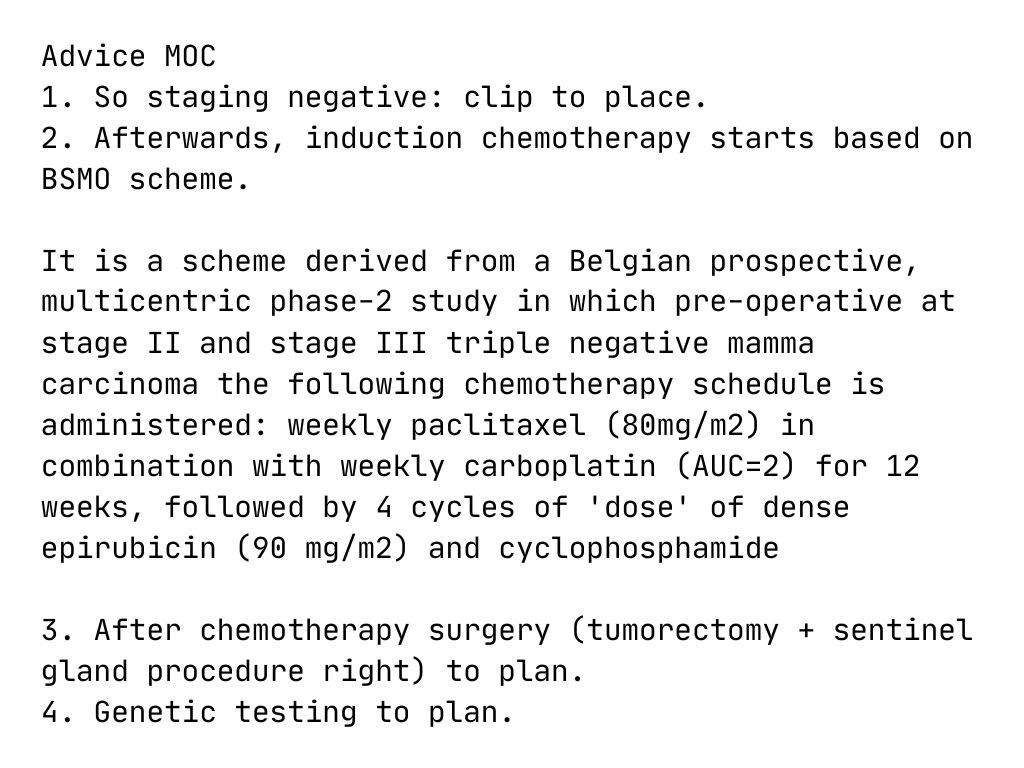
multidisciplinary oncology consultation
In the meantime, the multidisciplinary oncology consultation took place at the hospital. Radiologists, oncologists, radiotherapists, gynecologists, they all sat together to discuss, amongst others, also my case.
what was the verdict? what therapy plan they were going to propose to me? It’s all in a letter which I translated to English, redacting privacy information and trimming it down to the essential core. Believe it or not: my entire future depended on this plan.
Please note I have not translated this very well. I don’t need to, and I don’t want to.
October 27, 2023
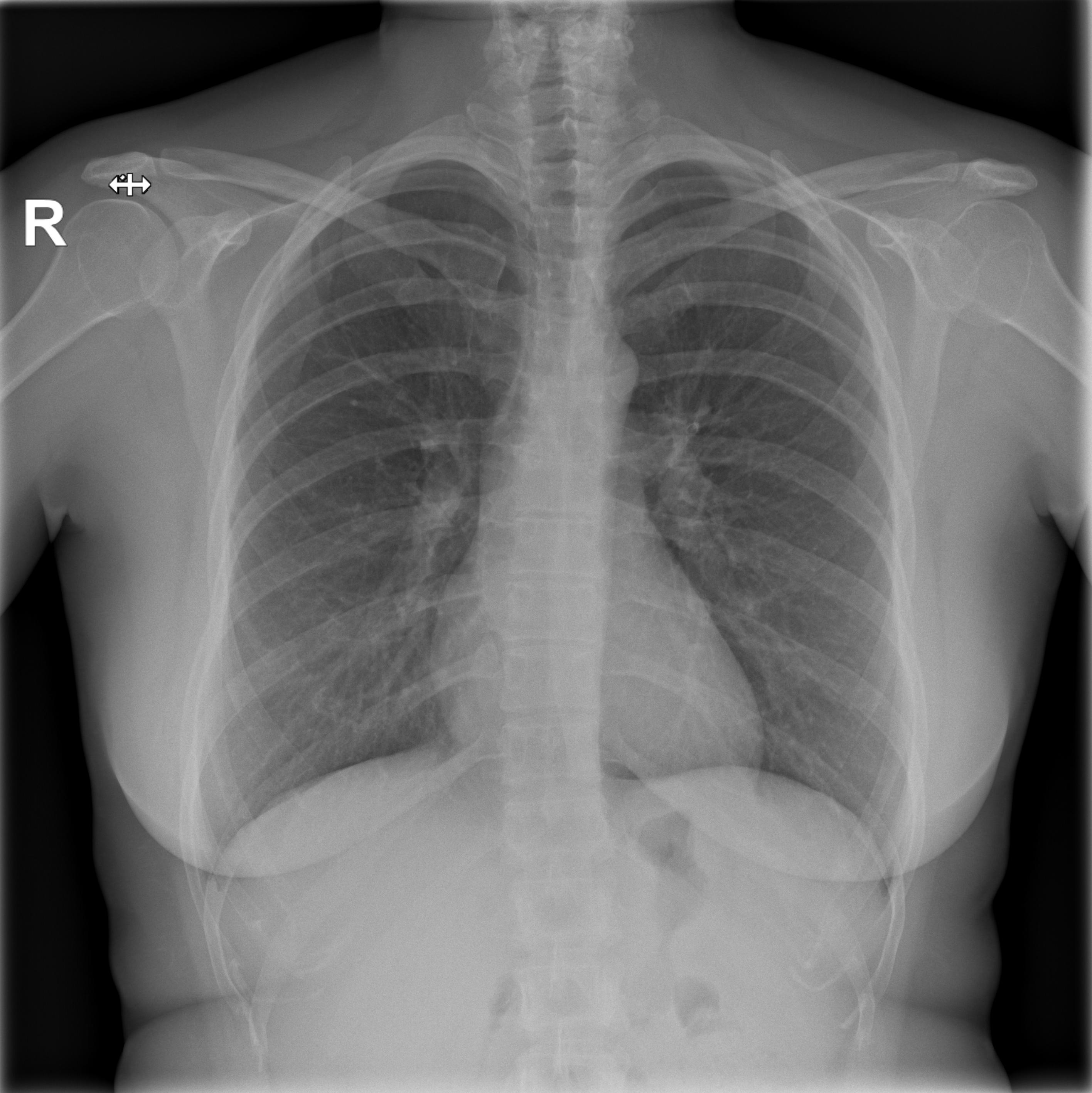

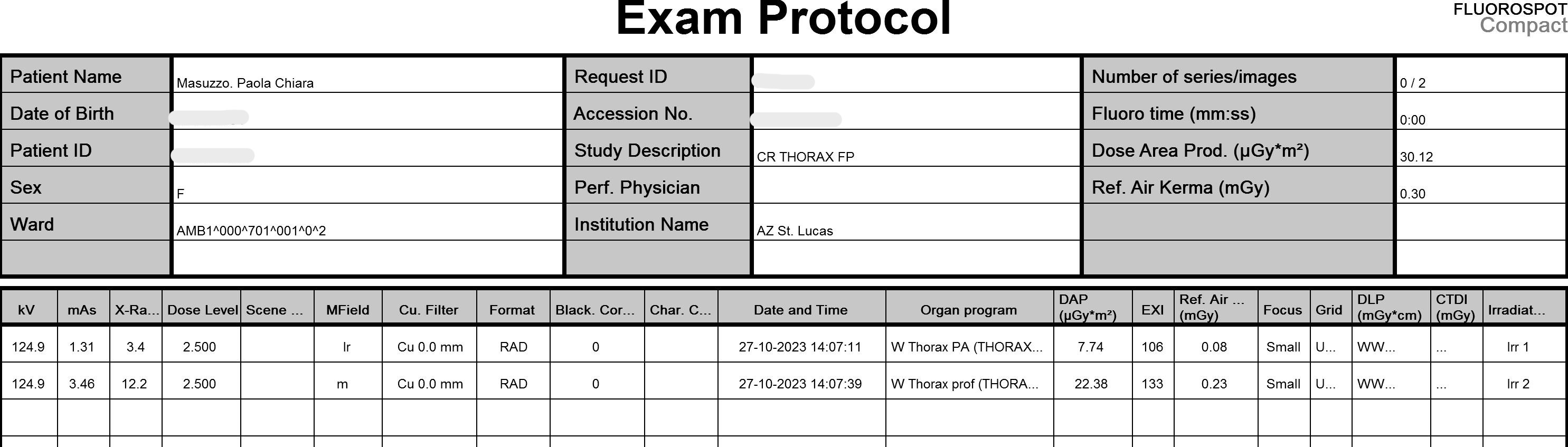
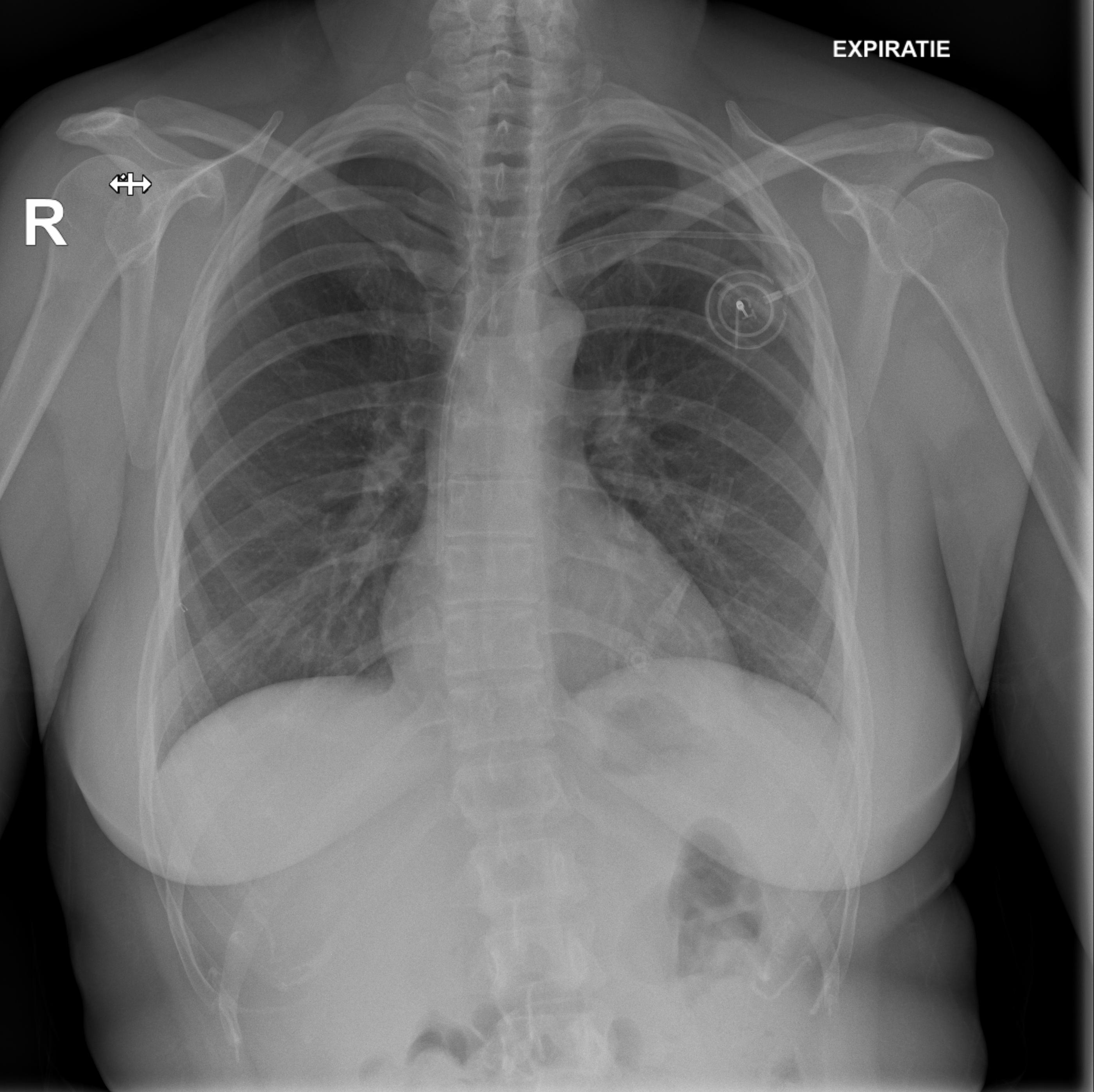
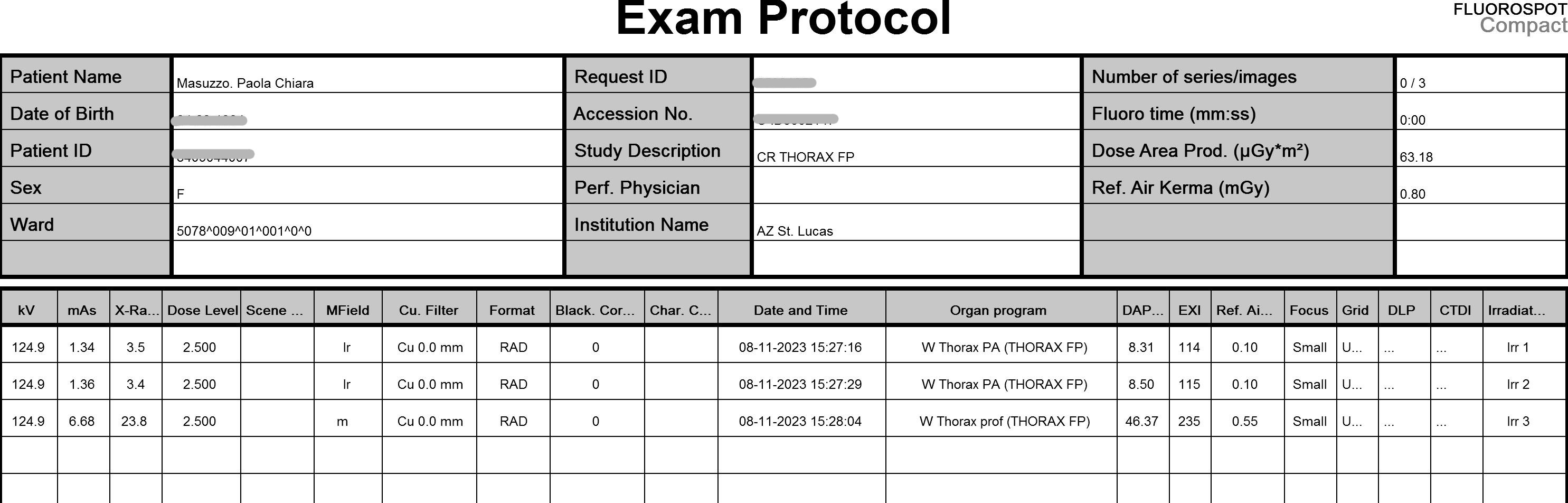
chest x-ray
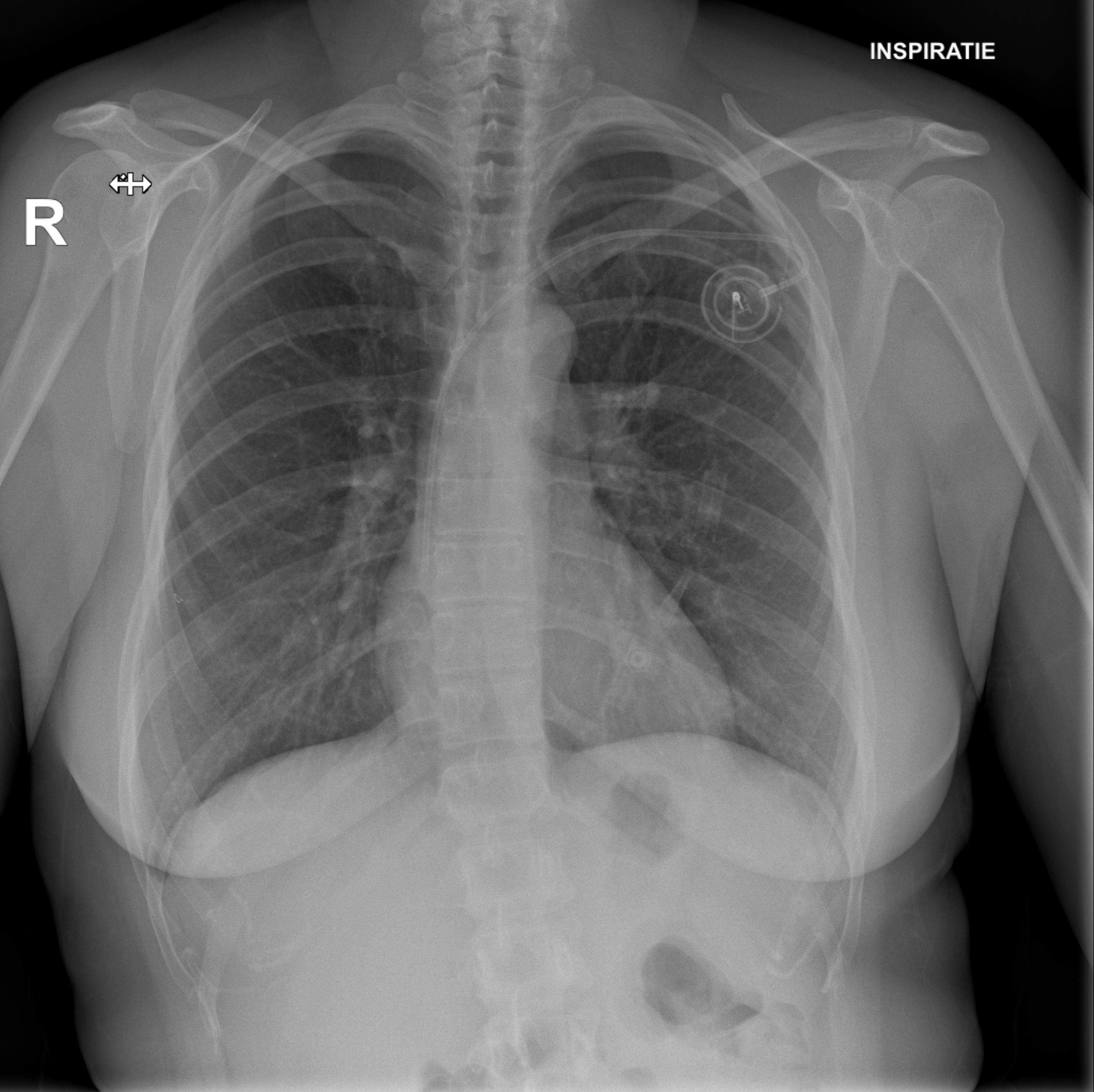
The medical checkups continued, and a few things happened on October 27th. I had a chest radiology exam, which showed that no pulmonary lesions were present or suspected. Another piece of the puzzle falling into place.
I included the two x-ray images, along with a recap of the protocol they used for the exam. I will be honest, I don’t understand it (all), but I couldn’t help but thinking that this is data that plays a crucial role, too: a different protocol might have shown things differently? more of it, less of it?

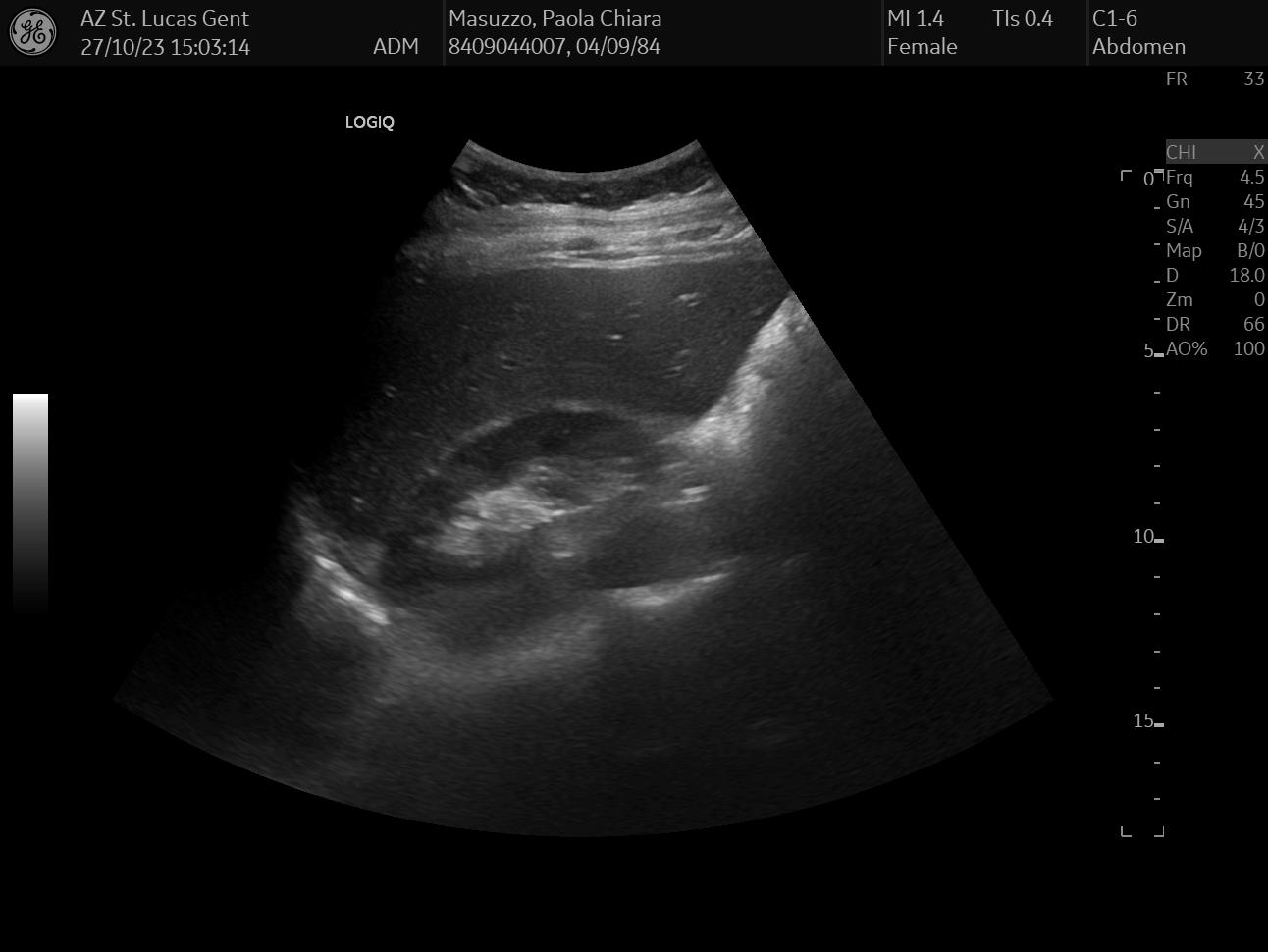

ultrasound liver, gallbladder, bile duct
On the same day, I also had an abdomen ultrasound of my liver, gallbladder, and bile duct, which together can paint a pretty accurate status of your hepatic health - or lack thereof.
Like with any ultrasound exam carried over by a physician, the visit was pretty painless and I got the results on the spot: everything looked pretty normal. The 3 images I selected from this exam are pretty random: I chose the ones that looked the funniest to me, but I honestly have no idea what they mean.
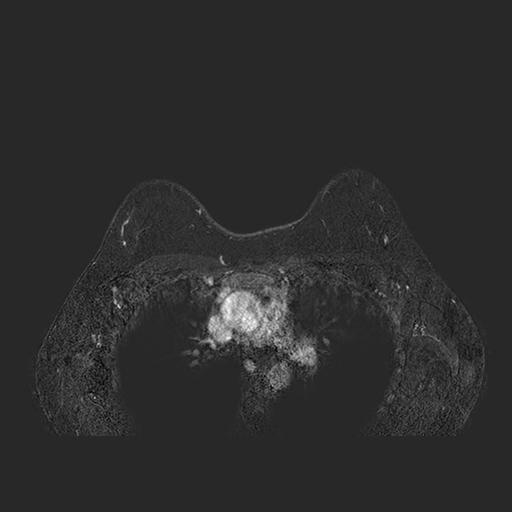
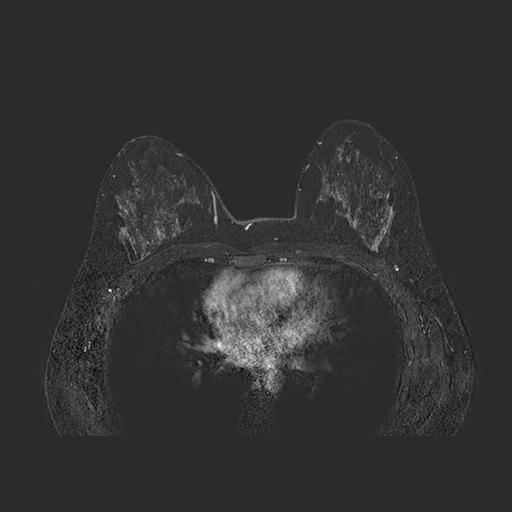

first magnetic resonance
To close off this day, I also did a magnetic resonance imaging (MRI) exam with a contrast medium. The question to answer here was mainly: was my tumor a solitary lesion? or part of a bigger, scattered group? and were my axillary lymph nodes healthy or not? This is the imaging modality for dense breast imaging: it’s also, unfortunately, very expensive.
The doctors panicked here a little bit, as the MRI showed weird inflammatory activities around my axillary zones: it turned out this was due to the double shots of vaccine I had 24 hours before (both for COVID and for the seasonal flu). Admittedly not a great timing, but I needed to help my immune system as fast as possible before starting chemotherapy. Yes, those up there are my boops.
November 01, 2023
first appointment with my oncologist
On this day I met my oncologist for the first time.
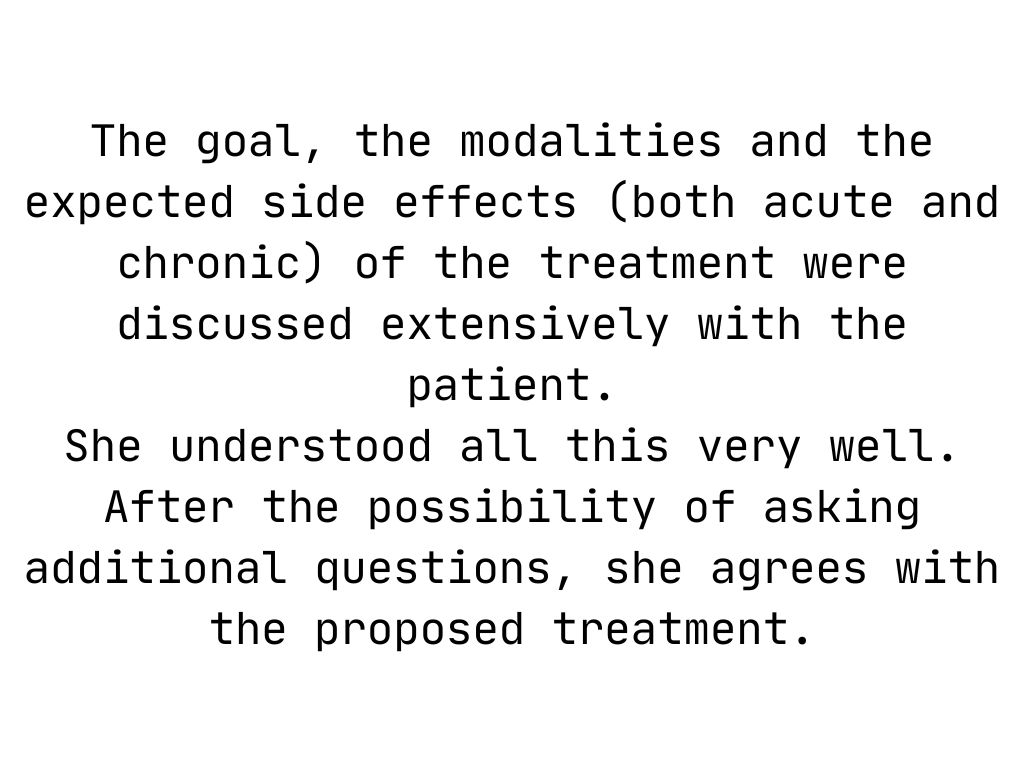
I think I spent most of the appointment crying, first, and asking questions, afterwards. They explained - again, and in a greater amount of detail - the therapy plan, the steps still required for the actual plan to start, the side effects, and the overall goal we were trying to achieve: slow down the tumor proliferation, and hopefully kill it all.
You will lose all your hair, and it’s going to happen very, very fast.
I have a full report from this appointment, and a list of questions I asked the doctor along with the answers I received. I am still not sure if I want to share this in great detail, so for now I just took the report, extracted the very last bit of it and translated it to English. I think you can appreciate that it kind of reflects well the type of oncological patient I have always been: curious, communicative, participating. The hospital and my doctors have always respected my autonomy and encouraged me to exercise full agency during my treatment.
November 02, 2023
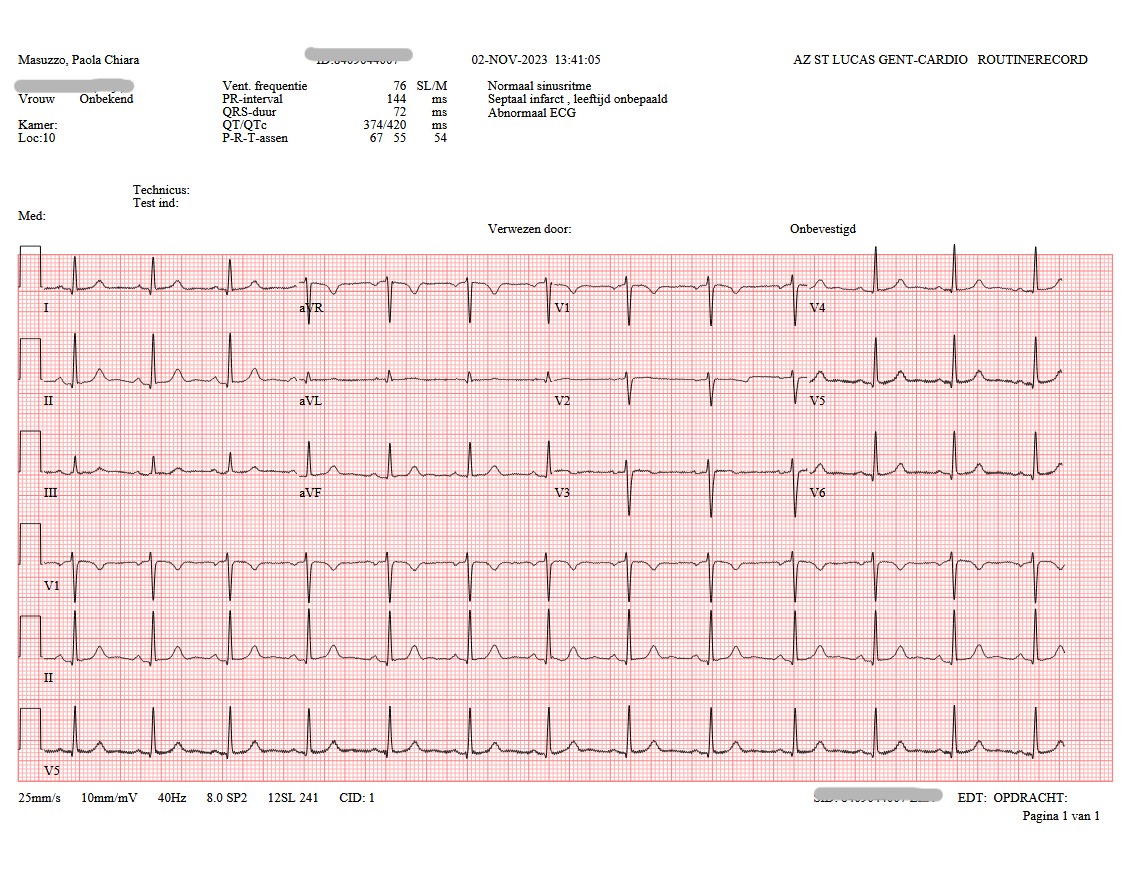
cardiological check in preparation of chemotherapy
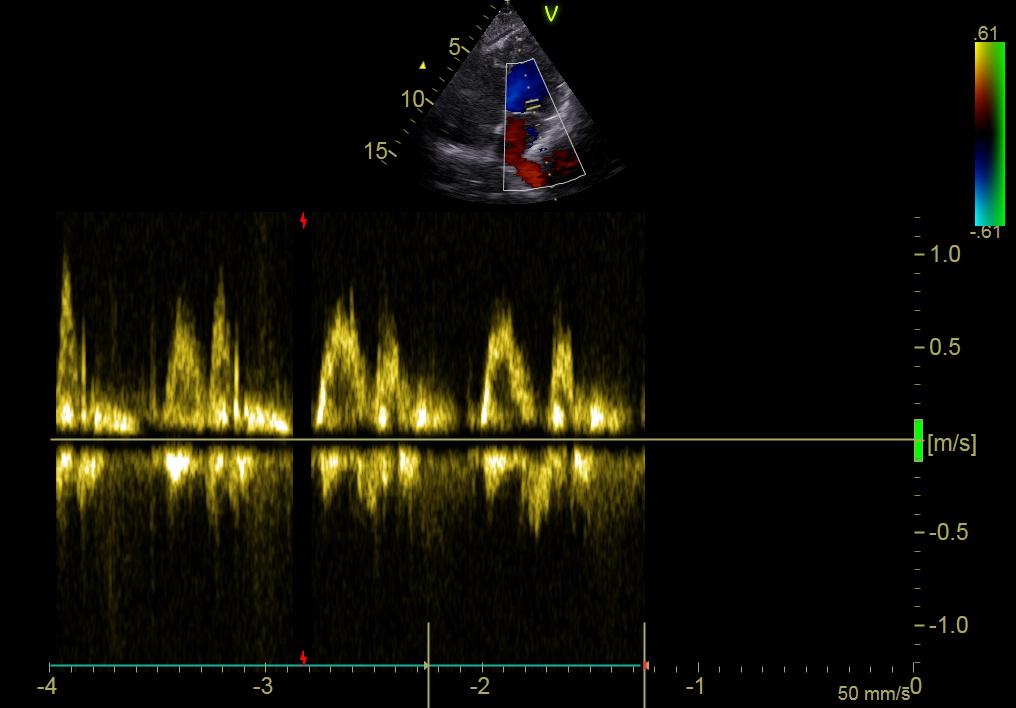
Before starting chemotherapy, we needed to make sure my heart was healthy enough to endure it. So I went to the hospital for a full cardiological exam: an electrocardiogram followed by an echography. We didn’t expect anything to show up - have never suffered from cardiological issues - but basically, like with everything, “you never know”.
The echocardiogram is used to highlight the structure, function, and blood flow of the heart. The second image shows a color flow doppler, with in blue the blood that flows from the probe and in red the blood that flows towards it.
November 06, 2023


breast clip insertion
At this point of the ordeal we still needed to take care of two things, and both of these had to do with implanting stuff in my body. The first thing we inserted was a little clip in my breast, a tiny titanium marker used to pinpoint the exact position of the tumor. If we were going, hopefully, to kill the whole tumor, the cli was going to guide the surgeon find the correct area for removal later on. Furthermore, the clip was going to be monitored during imaging exams in the course of chemotherapy to understand changes over time.
This procedure happens with the same principle of a biopsy: a needle is inserted in the breast, but instead of taking sample away, the needle leaves the small clip behind. In the records I have selected from this procedure you can see the lesion in my breast, the long needle inside it, and eventually the clip in the middle of the tumor.
November 07, 2023

surgery to implant my port-a-cath
The very last thing before chemotherapy could start was the insertion of a port-a-cath in my body. A port is an implantable device that allows long-term central venous access, very useful for administering medications like chemotherapy, for drawing blood, or for providing intravenous fluids. With an implanted port, the medicine goes straight to a central vein, bypassing smaller, peripheral veins, and protecting them from damage.
I received my port-a-cath with local anestesia: surgery started at 12:32pm and finished at 13:12pm. The x-ray image I have uploaded shows the port in place during surgery. I have called my port-a-cath Portia - very clever, I know.
Two years later it’s still in my body. One day I’ll bid it goodbye, I think (hope?).
November 08, 2023

first chemotherapy session
Chemotherapy day finally arrived: the sooner I started, the better, obviously. Not sure what happened on the day, but I fainted while getting ready. The pain from the port surgery, the tiredness, the stress of it all, I just went down on my face. My oncologist suspected a pneumothorax (a collection of air outside the lung but within the pleural cavity) so I was sent to radiology for some x-rays.
They checked my lungs during inspiration and expiration: you can clearly see Portia with the catheter getting into my subclavian vein.
Luckly enough, I didn’t have a pneumothorax, so we went ahead with chemotherapy.
I did 12 sessions of weekly therapy + 4 sessions of biweekly therapy.